Supporting Populations at Risk for Co-occurring Disorders
By Ina A. Ramos, Ph.D.
Senior Technical Associate, The MayaTech Corporation
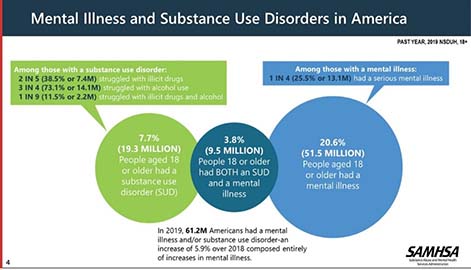
According to the SAMHSA 2019 National Survey on Drug Use and Health, 61.2 million Americans 18 and older reported having a mental and/or substance use disorder, a 6% increase from 2018.1 Mental illness and substance use disorders share common risk factors (e.g., genetic, epigenetic, environmental, stress, trauma, adverse childhood experiences); therefore, the impact of having a mental health or substance use disorder on brain structure can contribute to the development of another disorder.2 An individual with co-occurring disorders has at least one mental disorder and at least one substance use disorder. In 2019, 9.5 million adults (18 and older) reported having co-occurring disorders in the past year. Those between 18-25-years reported the highest rates of co-occurring disorders (7.6%) compared to those 26-49 years (5.2%) and 50 or older (1.5%). When examining the most commonly used substances among adults, illicit drugs had higher rates of use in the past year for those experiencing any mental disorder (38.8%) and a serious mental illness (49.4%), followed by marijuana at 32.5% and 39.8%, respectively.1
Certain populations experience a disproportionate burden of environmental risk factors (primarily stress) for co-occurring disorders leading to overrepresentation of these populations with co-occurring disorders, and underrepresentation in treatment for these disorders. Higher rates of co-occurring disorders have been reported in Blacks, Latinx, and LGBTQ populations, as well as people who are justice-involved, homeless, have disabilities, or lower income.3 COVID-19 has exacerbated co-occurring disorders for many people due to restrictions on service options, social isolation, loss of familiar daily structure, unemployment, financial stress, and disruption of services. This myriad of issues may cause increased levels of stress, which can lead to relapse, and an increased risk of contracting COVID-19, exacerbating existing issues for those who are most at need. It is anticipated that COVID-19 will cause substantial increases in substance use disorders, mental illness, and suicidality in all age groups.4
So, how do we begin to support those populations at greatest risk for co-occurring disorders? To find out, we sought advice from Dr. Brandy F. Henry, a clinical social worker who works to improve the health of criminalized populations with co-occurring disorders. Her publications describe the epidemiology of co-occurring disorders as related to exposure to stress and trauma, and best practices for interventions to address these disorders and more recently, the impact of the COVID-19 pandemic as an adverse experience. Dr. Henry coauthored a journal article entitled “ COVID-19, Mental Health, and Opioid Use Disorder: Old and New Public Health Crises Intertwine,” which examines opioid use disorder, mental health problems, trauma, and social and health disparities in the context of COVID-19. In a recent webinar, Dr. Henry provided the following best practices:
- Screening and Assessment
- Screen for both mental health and substance use disorders.
- Screen and assess for trauma and stress (historical and current).
- Identify relevant psychosocial factors (i.e., cultural background, barriers/facilitators to care, care preferences).
- Establish trust and rapport (mistrust and shame are common in this population and are often exacerbated by provider stigma, which includes intersecting forms of stigma and discrimination).
- Treatment
- Treat mental health and substance use disorders together (integrated services).
- Tailor the treatment to the person’s specific needs (symptoms, diagnosis, psychosocial factors).
- Apply trauma informed, gender and culturally appropriate practices to establish safety and promote trust.
- Use evidence-based practices – treatment may require a combination of behavioral and medication therapies (effective medications exist for opioid, alcohol, and nicotine use disorders).
- Recovery
- Recognize that recovery is a long-term process where people with co-occurring disorders regain health and social function (does not necessarily include abstinence).
- Develop a relapse prevention plan that addresses both mental health and substance use symptoms and includes long-term supports.
- Connect patients to peer recovery and mutual support programs.
SAMHSA Resources
To address these issues, SAMHSA continues to develop advisories, treatment improvement protocols, and resource guides that address co-occurring disorders. In addition, it provides prevention programs such as the Technology Transfer Centers (TTC) and Clinical Support System for Serious Mental Illness (SMI Adviser). The TTC develops and strengthens the specialized behavioral healthcare and primary healthcare workforce that provides prevention, treatment, and recovery support services for substance use disorders and mental illness. The SMI Adviser initiative supports the use and implementation of evidence-based screening and treatment for serious mental illness through education and consultation.
- First-Episode Psychosis and Co-Occurring Substance Use Disorders, Evidence-Based Resource Guide Series, October 2019.
- This guide contains a foreword and five chapters designed to be brief and accessible to healthcare providers, healthcare system administrators, community members, and others working with individuals at risk for, experiencing, or recovering from a substance use disorder and/or mental illness. This guide reviews the literature, provides research-based recommendations for practice, and provides implementation examples by first-episode psychosis treatment programs.
- Substance Use Disorder Treatment for People with Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series, No. 42, March 2020.
- This Treatment Improvement Protocol (TIP) update is intended to guide counselors and other addiction professionals sequentially through the primary components of proper identification and management of co-occurring disorders. This TIP is divided into eight chapters designed to thoroughly cover all relevant aspects of screening, assessment, diagnosis, treatment, and programming.
- Substance Use Disorder Treatment for People with Co-Occurring Disorders, Advisory, March 2021.
- This Advisory is based on SAMHSA’s TIP 42 (see above), and highlights (in brief) strategies for counselors and administrators to properly screen, assess, diagnose, and manage the treatment of individuals with co-occurring disorders.
References
- https://store.samhsa.gov/product/key-substance-use-and-mental-health-indicators-in-the-united-states-results-from-the-2019-national-survey-on-Drug-Use-and-Health/PEP20-07-01-001
- https://www.drugabuse.gov/publications/research-reports/common-comorbidities-substance-use-disorders/why-there-comorbidity-between-substance-use-disorders-mental-illnesses
- https://mfpwebinars.s3.us-east-1.amazonaws.com/co-occurring-disorders/508_MFPCC_Co-occurring_Disorders_26May2021_TRANSCRIPT.pdf
- https://www.samhsa.gov/data/sites/default/files/reports/rpt29392/Assistant-Secretary-nsduh2019_presentation/Assistant-Secretary-nsduh2019_presentation.pdf
